When Scott Davis first heard the words “lung cancer,” he didn’t panic. Instead, he and his wife Kerri leaned into their faith, trusted their care team, and embraced the cutting-edge technology that helped catch his cancer early and treat it with precision.
Davis, 72, a retired letter carrier lives in Overbrook, Kansas, with his wife, Kerri – proud parents of four sons, grandparents to 11, and great-grandparents to one—with another great-grandchild on the way. “We’ll be 24 strong soon,” he said with a smile.
His cancer journey began in April 2025, when a routine chest X-ray revealed a suspicious mass. Within days, Davis was connected with Abhishek Chakraborti, MD, a pulmonologist at The University of Kansas Health System St. Francis Campus in Topeka. What followed was a whirlwind of swift, coordinated care.
Ion bronchoscopy
“From the time of the CT scan to the biopsy and then meeting with oncology, it was just ten business days,” he said. “We were pretty surprised ourselves how fast it was.”
The speed of care was just the beginning. What truly set Davis’s experience apart was the use of advanced artificial intelligence (AI) and robotic technology. The hospital is the first in Topeka to use AI-powered software called Eon to enhance radiology and detect suspicious lung nodules—often found incidentally during scans for other conditions.
“This technology adds an extra layer of diagnostic insight,” Dr. Chakraborti explained. “It flags potentially cancerous findings that might otherwise go unnoticed.”
Davis and Kerri were initially hesitant about undergoing a biopsy, given their family history with cancer. “We weren’t really fond of the idea,” he admitted. “Back in the day, biopsies were hit or miss. But Dr. Chakraborti explained the capabilities of the new Ion bronchoscopy, and we were amazed.”
Ion bronchoscopy is a robotic-assisted procedure that allows physicians to reach deep into the lungs with remarkable precision. “They could get so close to the tumor, it made the biopsy much more accurate,” Davis said.
Kerri added, “The most miraculous thing was how they were able to get tissue from a lymph node that didn’t even show up on the scans. It was so tiny, they wouldn’t have found it without the Ion technology. That’s what really made us feel confident—we knew they were catching everything.”
Questions, answers and confidence
That confidence only grew during their first meeting with Dr. Chakraborti. “He spent 45 minutes to an hour with us, answering every question,” Davis said. “We walked out of there feeling completely secure. We had 100% confidence.”
Following the biopsy, Scott met with oncologist Osama Diab, MD, who laid out a comprehensive treatment plan. It included a PET scan, MRI, chemotherapy, and radiation therapy. The radiation oncologist used advanced computer mapping to target the tumor with pinpoint accuracy, minimizing exposure to surrounding organs.
“They showed us how the radiation would stop before hitting my heart,” Davis said. “It was amazing. They even targeted the lymph node on the right side, even though the tumor was on the left.”
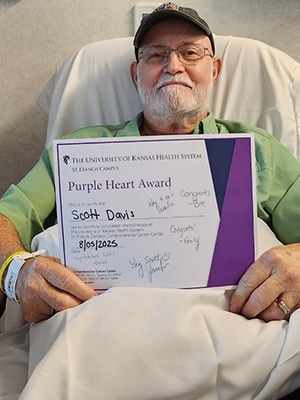
Scott was also accepted into a five-year clinical trial to test a more targeted and shorter radiation regimen. “Instead of six weeks, I did five,” he said. “They gave a higher dose to the tumor area, a lower dose to the lymph node, and a middle dose in between—because they figured the cancer had to travel somehow.”
He began chemotherapy and radiation on July 7, receiving radiation five days a week and chemo once a week. His last chemo treatment was on August 11. In September, he started immunotherapy, a newer treatment that uses the body’s immune system to fight cancer.
“Dr. Diab explained that surgery wasn’t an option after radiation, but immunotherapy could be just as effective,” Scott said. “It’s once a month for a year, and so far, everything looks positive.”
In fact, a CAT scan performed shortly after chemo showed noticeable shrinkage in the tumor—earlier than expected. “Our oncologist was surprised,” Davis said. “He took it as a very good sign.”
Throughout the process, Scott and Kerri never lost faith. As devout Christians, they believe in the healing power of Jesus Christ. “But we also believe God created doctors for a reason. After meeting this team, we had no doubts. They were fantastic—from the doctors to the nurses to the APRNs.”
Everyone knew his name
The University of Kansas Health System Cancer Center at St. Francis Campus became a second home. “They treat you like family,” Davis said. “The receptionist knows me by name. I just walk off the elevator and she’s already got me checked in.”
Outside of treatment, Scott and Kerri remain active in their church. Davis serves as a building administrator, handling everything from furnace filters to lawn care. Kerri leads the hospitality ministry. Together, they help organize worship nights and community meals.
As Davis continues immunotherapy, he remains hopeful and grateful. “We’ve got a church full of gray-haired little old ladies praying for me,” he said with a chuckle. “And we’ve got the best care team we could ask for.”
For Scott and Kerri, facing lung cancer wasn’t just about surviving, it was about trusting, connecting, and giving back. And thanks to a blend of faith, family, and technology, they’re doing just that.
Did you know that November is Lung Cancer Awareness Month? For more information on Ion and our lung screening and nodule program, click here. If you have any questions, please reach out to our lung nodule coordinator at (785) 295-8377.


